
Diabetes is a chronic condition that can have significant implications for wound healing. This article will explore the key mechanisms by which diabetes impairs the body’s ability to effectively heal wounds, leading to an increased risk of chronic, non-healing wounds. We will delve into the various factors that contribute to delayed wound healing in diabetes, including impaired blood circulation, neuropathy, and compromised immune response. Additionally, we will discuss the management and treatment of diabetic wounds, as well as strategies for preventing wound healing complications.
Read interesting things at : luoghievisioni
Key Takeaways
- Diabetes can significantly impair the body’s wound healing process, leading to an increased risk of chronic, non-healing wounds.
- Impaired blood circulation, neuropathy, and compromised immune response are key factors contributing to delayed wound healing in diabetes.
- Diabetic foot ulcers are a common and serious complication of diabetes, often leading to severe consequences if left untreated.
- Effective management of diabetic wounds requires a multifaceted approach, including strict glycemic control, appropriate wound care, and the utilization of adjunctive therapies.
- Proactive prevention strategies, such as regular foot care and lifestyle modifications, can help reduce the risk of wound healing complications in individuals with diabetes.
Understanding Diabetes and Its Impact on Wound Healing
Diabetes is a chronic metabolic disorder characterized by high blood sugar levels (hyperglycemia) due to the body’s inability to produce or effectively use insulin, a hormone responsible for regulating blood glucose. This condition can have significant implications for wound healing, as it can disrupt the body’s natural processes and increase the risk of complications.
What is Diabetes?
Diabetes is a chronic condition that occurs when the body either does not produce enough insulin or is unable to effectively use the insulin it produces. Insulin is a hormone that regulates blood sugar levels, and its absence or ineffectiveness leads to a sustained state of hyperglycemia, or high blood sugar.
Types of Diabetes
There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is an autoimmune condition where the body does not produce insulin, while type 2 diabetes is the more common form, where the body becomes resistant to insulin or does not produce enough of it.
Complications of Diabetes
Complications of diabetes can include nerve damage (neuropathy), impaired circulation, and a weakened immune system, all of which can significantly impact wound healing. These complications can lead to delayed wound healing, increased risk of infection, and the development of chronic, non-healing wounds, such as diabetic foot ulcers.
Delayed Wound Healing in Diabetes
One of the significant challenges faced by individuals with diabetes is the delayed healing of wounds. This phenomenon can be attributed to several factors, including impaired blood circulation and neuropathy with reduced sensation.
Impaired Blood Circulation
Diabetes can lead to a common complication known as impaired blood circulation. This condition reduces the delivery of oxygen and essential nutrients to the wound site, hindering the body’s natural healing process. As a result, diabetic wounds may take longer to heal, increasing the risk of complications such as infection and further tissue damage.
Neuropathy and Reduced Sensation
Another factor contributing to delayed wound healing in diabetes is neuropathy and reduced sensation. Diabetes can cause nerve damage, leading to a decrease in the individual’s ability to feel pain or discomfort. This reduced sensation can make it challenging for people with diabetes to detect injuries or notice the development of wounds, leading to delayed treatment and a higher risk of infection.
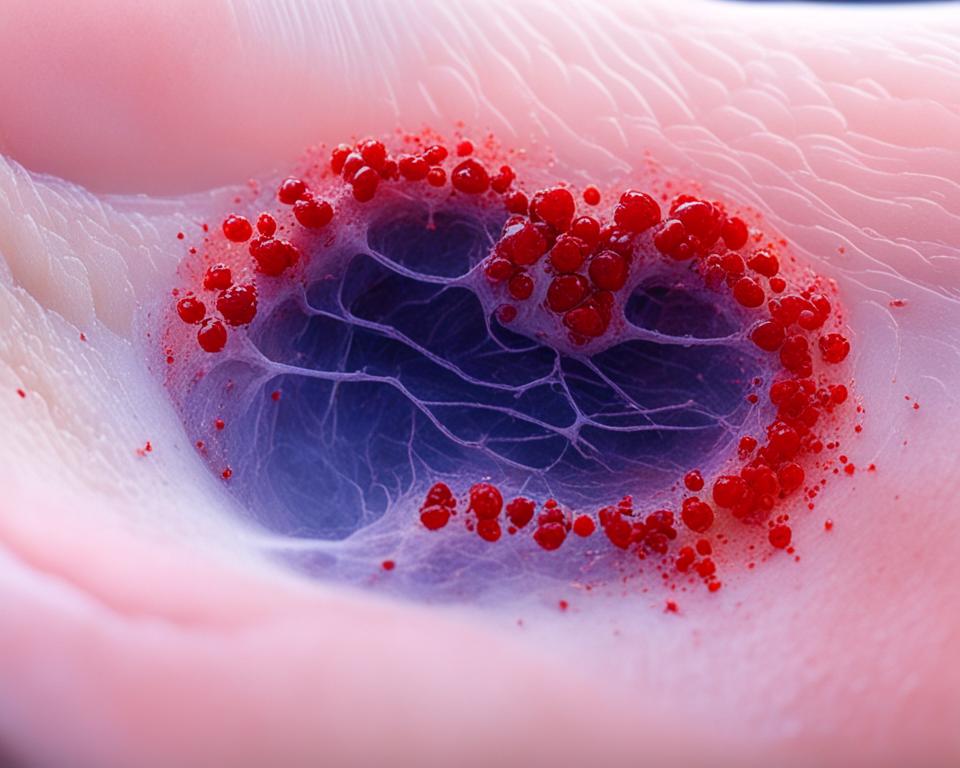
Diabetic Foot Ulcers
Diabetic foot ulcers are a common and serious complication of diabetes, often occurring due to a combination of factors, including impaired circulation, neuropathy, and trauma. Individuals with diabetes have an increased risk of developing these types of wounds, which can lead to severe complications if left untreated.
Risk Factors for Diabetic Foot Ulcers
Several factors can contribute to the development of diabetic foot ulcers, including poor blood circulation, nerve damage (neuropathy), and a history of previous foot ulcers or amputations. Individuals with diabetes who have uncontrolled blood sugar levels, are overweight or obese, and do not engage in proper foot care are at an increased risk of developing these types of wounds.
Potential Complications of Diabetic Foot Ulcers
If left untreated, diabetic foot ulcers can lead to serious complications, such as infection, gangrene, and even amputation. Infections can quickly spread, leading to more severe issues, while gangrene, or the death of tissue, can necessitate the removal of the affected limb to prevent the spread of the condition. Prompt and effective management of diabetic foot ulcers is crucial to prevent these devastating outcomes.
Impaired Wound Healing in Diabetes
Diabetes can significantly impair the body’s natural wound healing process through several complex mechanisms. One of the key factors contributing to impaired wound healing in diabetes is the compromised inflammatory response.
Impaired Inflammatory Response
The inflammatory response is a crucial initiator of the wound healing cascade, but in individuals with diabetes, this response is often delayed or insufficient. Hyperglycemia, a hallmark of diabetes, can disrupt the normal signaling pathways and the recruitment of inflammatory cells to the wound site, leading to a suboptimal inflammatory reaction that hinders the subsequent stages of wound repair.
Reduced Collagen Production
Diabetes can also impair the production of collagen, a vital structural protein essential for wound repair. Collagen provides the framework for tissue regeneration and wound closure, but in diabetic individuals, reduced collagen production can result in delayed and impaired wound healing.
Decreased Angiogenesis
Another significant factor contributing to impaired wound healing in diabetes is the decreased formation of new blood vessels, known as angiogenesis. Adequate blood supply is crucial for delivering oxygen and nutrients to the wound site, facilitating the various stages of healing. However, diabetes can disrupt the angiogenic processes, leading to decreased angiogenesis and compromised wound healing.
By understanding these key mechanisms of how diabetes impairs the body’s natural wound healing capabilities, healthcare providers can develop targeted interventions and strategies to address the unique challenges faced by individuals with diabetes in the management of wounds and the prevention of chronic, non-healing wounds.
How Diabetes Affects Wound Healing
Diabetes can negatively impact the how diabetes affects wound healing through various pathways, including impaired blood circulation, nerve damage, compromised immune function, and disruptions in the normal wound healing process. These factors can lead to delayed healing, increased risk of infection, and the development of chronic, non-healing wounds, such as diabetic foot ulcers.
One of the primary ways how diabetes affects wound healing is through impaired blood circulation. Diabetes can damage the blood vessels, reducing the delivery of oxygen and nutrients to the wound site, which are essential for the healing process. This can result in delayed wound healing and an increased risk of infection.
Additionally, how diabetes affects wound healing is also influenced by nerve damage, or neuropathy, a common complication of diabetes. Neuropathy can reduce sensation in the affected areas, making it difficult for individuals with diabetes to detect injuries or feel pain, leading to delayed treatment and increased risk of infection.
Furthermore, diabetes can compromise the immune system, how diabetes affects wound healing by impairing the body’s ability to fight off infections and properly respond to the wound healing cascade. This can lead to a prolonged inflammatory response and disruptions in the normal wound healing process.
“Diabetes can negatively impact wound healing through various pathways, including impaired blood circulation, nerve damage, and compromised immune function.”
The combination of these factors can result in delayed wound healing, increased risk of infection, and the development of chronic, non-healing wounds, such as diabetic foot ulcers, which can have serious consequences if left untreated.
Diabetes Wound Care
Effective diabetes wound care is crucial for individuals with diabetes to promote healing and prevent complications. Proper wound management involves maintaining a moist wound environment, using appropriate dressings, and implementing offloading techniques to reduce pressure on the affected area.
Importance of Proper Wound Management
Maintaining a moist wound environment and using the right dressings can significantly enhance the healing process for individuals with diabetes. Wound dressings that are tailored to the specific needs of the wound, such as absorbing exudate or providing a barrier against infection, can help create an optimal healing environment.
Offloading and Pressure Relief
One of the key aspects of diabetic wound care is the implementation of offloading techniques to reduce pressure on the affected area. This is particularly important for the management of diabetic foot ulcers, as pressure on the foot can impede healing and lead to further complications.
The use of specialized footwear, such as offloading boots or custom-made shoes, can help redistribute pressure and prevent the development of new ulcers. Additionally, the application of pressure relief devices, like wheelchair cushions or mattress overlays, can be beneficial for individuals with diabetes who are at risk of developing pressure ulcers.
By implementing appropriate offloading and pressure relief strategies, individuals with diabetes can promote the healing of existing wounds and reduce the risk of future complications, ultimately improving their overall wound care outcomes.
Diabetes and Chronic Wounds
Diabetes can also increase the risk of developing chronic, non-healing wounds, such as venous leg ulcers and pressure ulcers. These types of chronic wounds pose a significant challenge for individuals with diabetes and require specialized care and management.
Venous Leg Ulcers
Venous leg ulcers are a common type of chronic wound that often affects individuals with diabetes. These ulcers are caused by poor circulation in the veins, a condition that is further exacerbated by the vascular complications associated with diabetes. Individuals with diabetes are more susceptible to developing venous leg ulcers due to the impaired blood flow and reduced ability to effectively heal these wounds.
Pressure Ulcers
Pressure ulcers, also known as bedsores, are another type of chronic wound that individuals with diabetes are at an increased risk of developing. These wounds occur due to sustained pressure on specific areas of the body, often in individuals who are immobile or confined to a bed or wheelchair. Diabetes can contribute to the development of pressure ulcers by reducing blood flow and impairing sensation, making it difficult for the individual to feel or detect the pressure buildup that leads to these chronic wounds.
Diabetes Slows Wound Repair
Diabetes can significantly impact the wound repair process by disrupting various cellular and physiological mechanisms. Diabetes slows wound repair through a combination of impaired cellular processes and a compromised immune response.
Impaired Cellular Processes
Hyperglycemia, or high blood sugar levels, associated with diabetes can disrupt the normal functioning of cells involved in wound healing. This includes impaired migration and proliferation of these critical cells, hindering their ability to effectively close and repair the wounded area.
Compromised Immune Response
Diabetes can also compromise the body’s immune system, reducing its capacity to fight off infections and properly respond to the wound healing cascade. This compromised immune response can further delay the wound repair process and increase the risk of complications, such as wound infections.
By understanding the ways in which diabetes slows wound repair through impaired cellular processes and a compromised immune response, healthcare professionals can better develop targeted interventions and strategies to support wound healing in individuals with diabetes.
Diabetes Wound Healing Complications
Individuals with diabetes face an elevated risk of developing complications related to wound healing, particularly infections and amputations. Impaired circulation and a compromised immune system can significantly increase the susceptibility to bacterial and fungal infections in diabetic wounds. If these infections are left uncontrolled or the wound healing process is severely impaired, it can ultimately lead to the need for amputation, a devastating outcome for those living with diabetes.
Infection
The combination of reduced blood flow and a weakened immune response in individuals with diabetes can make them more prone to developing infections in their wounds. These infections, if not properly managed, can rapidly worsen and lead to serious complications, such as sepsis or gangrene. Prompt recognition and treatment of any signs of infection, including redness, swelling, pain, or fever, are crucial for preventing further complications and promoting healing.
Amputation
In severe cases, when diabetic wounds fail to heal or become complicated by uncontrolled infections, amputation may become a necessary intervention. Diabetes is a leading cause of non-traumatic lower-limb amputations, often due to the development of diabetic foot ulcers that progress to the point of requiring removal of the affected limb. Proactive prevention, early intervention, and comprehensive wound management are essential to reduce the risk of this devastating complication for individuals with diabetes.
Diabetic Wound Management
Effective management of diabetic wounds involves a multifaceted approach, including strict glycemic control, the use of appropriate wound dressings and topical treatments, and the incorporation of adjunctive therapies. Maintaining optimal blood sugar levels is crucial for promoting wound healing, as hyperglycemia can impair the body’s natural healing processes.
Glycemic Control
Strict control of blood glucose levels is a critical component of diabetic wound management. Hyperglycemia, or high blood sugar, can significantly hinder the wound healing process by disrupting cellular functions, impairing immune response, and inhibiting the production of essential proteins like collagen. By achieving and maintaining glycemic control, individuals with diabetes can create an environment that is conducive to wound healing.
Wound Dressings and Topical Treatments
The selection and application of appropriate wound dressings and topical treatments can also play a vital role in supporting the healing of diabetic wounds. Dressings that maintain a moist wound environment, provide protection, and promote debridement can help create the optimal conditions for wound closure. Additionally, the use of topical antimicrobials, growth factors, and other specialized treatments may be necessary to address specific wound characteristics and facilitate the healing process.
Adjunctive Therapies
In some cases, the incorporation of adjunctive therapies may be utilized to enhance wound healing in individuals with diabetes. These therapies may include negative pressure wound therapy, which uses controlled suction to remove exudate and promote granulation tissue formation, or hyperbaric oxygen therapy, which delivers high concentrations of oxygen to the wound site to improve oxygenation and support the body’s natural healing mechanisms.
Diabetic Wounds Treatment
The treatment of diabetic wounds often requires a multidisciplinary approach, involving collaboration among healthcare professionals such as primary care physicians, podiatrists, wound care specialists, and other relevant specialists. This comprehensive approach helps address the various underlying factors that contribute to impaired wound healing in individuals with diabetes.
Multidisciplinary Approach
By working together, this team of healthcare providers can develop a personalized treatment plan that addresses the specific needs of the patient. This may include measures to improve glycemic control, implement appropriate wound care protocols, and address any underlying issues that may be hindering the healing process, such as circulatory problems or neuropathy.
Emerging Treatments
In addition to the multidisciplinary approach, ongoing research and clinical trials are exploring emerging treatments for diabetic wounds. These innovative solutions include advanced wound dressings, bioengineered skin substitutes, and regenerative therapies, which may offer new and promising avenues for managing this challenging condition.
By leveraging the expertise of a diverse healthcare team and staying abreast of the latest emerging treatments, healthcare providers can provide comprehensive and effective diabetic wounds treatment to their patients, improving outcomes and reducing the risk of complications.
Preventing Wound Healing Complications in Diabetes
Proactive prevention strategies are crucial for individuals with diabetes to reduce the risk of wound healing complications. This includes regular foot care and inspection to identify potential issues early, implementing lifestyle modifications such as maintaining optimal blood sugar levels and engaging in regular physical activity, and scheduling regular check-ups with healthcare providers to monitor overall health and wound healing status.
Foot Care and Inspection
Regular foot care and inspection are essential for individuals with diabetes to detect and address any potential issues before they escalate. This involves thoroughly examining the feet for any signs of injury, such as cuts, blisters, or calluses, and promptly addressing any concerns with a healthcare professional. Properly fitted, comfortable footwear and the use of protective devices, such as offloading pads or custom orthotic inserts, can help prevent the development of diabetic foot ulcers.
Lifestyle Modifications
Maintaining optimal blood sugar levels through a combination of diet, exercise, and medication management is a crucial step in preventing wound healing complications in diabetes. Engaging in regular physical activity can also improve circulation and promote overall wound healing. Additionally, adopting a healthy lifestyle, including a balanced diet, proper hydration, and stress management, can contribute to better overall health and wound healing outcomes.
Regular Check-ups
Scheduling regular check-ups with healthcare providers, such as primary care physicians, podiatrists, and wound care specialists, is essential for individuals with diabetes. These check-ups allow for the early detection and management of any emerging issues, as well as the monitoring of wound healing progress. By proactively addressing potential problems and making necessary adjustments to the treatment plan, individuals with diabetes can significantly reduce the risk of developing chronic, non-healing wounds.

Conclusion
In conclusion, diabetes can significantly impact wound healing through various mechanisms, including impaired blood circulation, neuropathy, compromised immune function, and disruptions in the normal wound healing process. Individuals with diabetes are at an increased risk of developing chronic, non-healing wounds, such as diabetic foot ulcers, which can lead to serious complications if left untreated.
Effective management of diabetic wounds requires a multidisciplinary approach, including strict glycemic control, appropriate wound care, and the utilization of adjunctive therapies. By understanding the key ways in which diabetes affects wound healing and implementing preventive strategies, such as regular foot care, lifestyle modifications, and maintaining regular check-ups, individuals with diabetes can reduce the risk of developing chronic wounds and improve their overall health outcomes.
Ultimately, addressing the complex interplay between diabetes and wound healing is crucial for healthcare professionals and patients alike. By staying informed and proactive, individuals with diabetes can take steps to mitigate the impact of this chronic condition on their wound healing process and work towards better overall health and quality of life.






